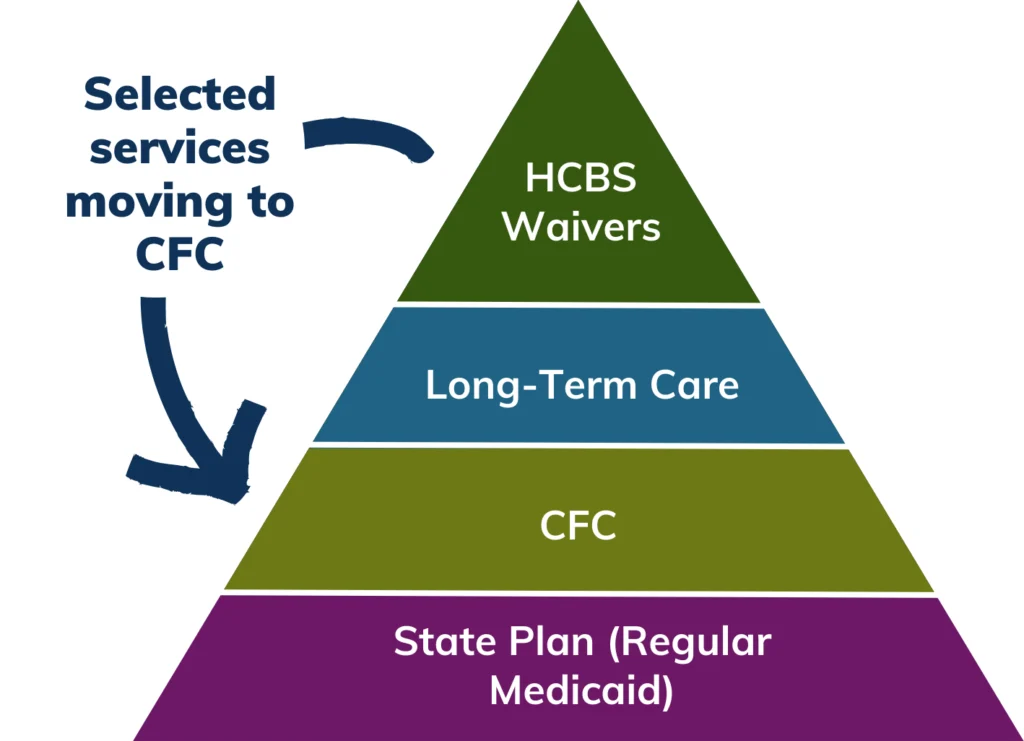
Now more individuals can receive support even if you’re not on a Medicaid Waiver.

More people can access care without needing to qualify for Medicaid waiver programs like SLS, CES, or EBD.
*Still need to meet level-of-care criteria
What are Attendant Supports
Attendant services provide hands-on, in-home support to individuals who need assistance with daily activities to live independently.
- This includes help with Activities of Daily Living (ADLs) such as bathing, dressing, grooming, eating, and mobility as well as Instrumental Activities of Daily Living (IADLs), which involve essential tasks like preparing meals, housekeeping, managing medications, and running errands.
These services are designed to enhance independence and quality of life by ensuring individuals receive the support they need in their home or community setting.
Supports available under CFC (moving out of HCBS waivers)
- Homemaker
- Personal Care
- Health Maintenance Activities
- Acquisition, Maintenance, and Enhancement of Skills (new federally required service)
- Remote Supports
- Remote Supports
- Technology
- Home Delivered Meals
- Transition Setup
- Electronic Monitoring
- Personal Emergency Response System
- Medication Reminders
Goal of CFC
Making HCBS accessible for more Medicaid members with expanded options and availability for self-directed care. See more on the Colorado Department of Health Care Policy & Financing (HCPF) CFC webpage.
How is CFC Funded?
CFC is a state plan option made possible by the Affordable Care Act, and it allows Colorado to enhance access to home and community-based services while benefiting from an increased federal match rate.
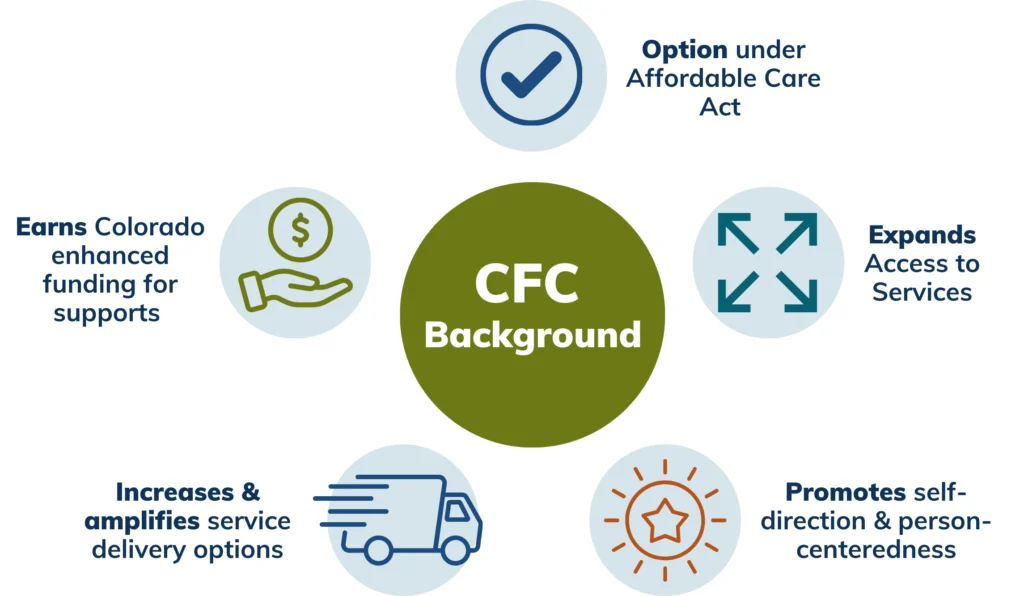
Why CFC Matters for Colorado
- Broader Service Access: More people can receive the supports they need without waiver restrictions.
- Increased Federal Funding: Colorado will receive an enhanced federal match for these services, improving long-term care funding.
- Better Integration: CFC creates a more streamlined, person-centered Medicaid system.
How Does CFC Benefit You?
For Members
Expanded Access: Receive services without needing to be enrolled in a Medicaid waiver.
More Choice & Control: CFC supports expanded self-directed service models such as Consumer-Directed Attendant Support Services (CDASS) and In-Home Support Services (IHSS). Members can hire, train, and manage their own attendants.
No Loss of Services: If currently receive services through a waiver, will not lose access—services are simply shifting to a new funding and delivery structure.
For Families
& Advocates
- Simplified Access: No need to navigate complex waiver eligibility criteria to receive essential attendant services.
- Increased Availability: More people can receive necessary care without waiver limitations.
- Enhanced Support Networks: CFC’s expanded model means aims to provide more community-based resources and better service continuity.
For Providers
- Increased Service Opportunities: Can support more members through state plan benefits; may see increased demand for services under CFC.
- Training & Guidance: Operational guidance and mandatory training will be provided to help navigate CFC’s implementation.
What Changes with CFC?
Key Takeaways
- Some services currently available only through Medicaid waivers will move under CFC, but will remain accessible to those who qualify.
- No duplication of services—if a member receives a service under a waiver, they cannot receive the same service under CFC.
- No age or disability-based differences—services and supports must be offered equitably across all eligible age groups and disabilities.
Resources + Next Steps
- Visit the dedicated HCPF CFC web page
- Check out the waiver comparison charts on the HCPF CFC Resources web page
- If you are already receiving case management from DP; your case manager will contact you when it is time to take action
- If you are not already receiving case management from DP, please visit our Get Started page
Key Milestones/Timeline
- July 1, 2025: Official launch of CFC in Colorado
- Gradual Transition: Current enrollees will transition gradually, ensuring service continuity.
- Ongoing Outreach: Training, resources, and support will be available for members, families and providers.
More Information
- Visit the official HCPF CFC web page for details
- Contact your case manager for personalized assistance.
- Community First Choice is a transformational step forward for Colorado’s Medicaid system. Stay informed, get involved, and be ready to embrace a more inclusive future for attendant services!
FAQs
What is CFC?
CFC is a new way of authorizing, delivering, and paying for certain services that have previously (mostly) only been available under Medicaid Waivers, including services like personal care and homemaker.
With CFC, more people can access care without needing to qualify for Medicaid waiver programs like SLS, CES, or EBD (while still needing to meet level-f-care criteria). More information is available in HCPF’s CFC FAQ.
Are current HCBS participants required to move to CFC?
Yes, if the participant is utilizing one of the services that are transitioning to CFC, they will transition, but there should not be any change in services.
This is primarily a back-end change that Case Managers will handle during the individuals’ annual service planning process. This affects everyone on a waiver accessing these services, except those on a DD waiver.
Will the process from referral to beginning services become shorter?
The process for referral could possibly be shorter if someone is only seeking CFC enrollment and not Long-Term Care Medicaid Waiver Enrollment. CFC-only enrollment does not require extra documents (medical documents, additional applications) to meet targeting criteria in order to qualify.
Is there a flow chart anywhere that identifies what goes under CFC and what goes under which waivers?
Please see the comparison chart links located under Department Guidance on HCPF’s website.
Who was previously ineligible before CFC but is now eligible?
Prior to CFC, individuals had to meet specific targeting criteria for a Medicaid waiver in order to qualify. For example, the CES waiver has targeting criteria that requires a child to need frequent intervention during the day and nighttime hours.
For current CFC services, an individual only needs to have eligible Medicaid and meet functional eligibility.
How does this program impact tasks that are currently under a Certified Nursing Assistant’s (CNA) responsibilities?
Through CFC, an individual is able to choose a provider to provide skilled and unskilled services without needing a CNA license. An individual may have a CNA and In-Home Support Services through CFC as long as services are not duplicative.
Does CFC change the tax exemption status of live-in caregivers? Public Partnerships, LLC (PPL), the Financial Management Service Provider for CDASS, states that CFC is not a waiver, resulting in a loss of tax exemption. Is this true?
HCPF is still waiting for guidance from the IRS on this topic. Please reference the informational memo, IM 25-018, by visiting HCPF’s 2025 Memo Series Communication page or by searching “IM 25-018” on HCPF’s website for additional information.
Will CFC free up some of the spending of the CES waiver budget because some of the services will be moving to CFC?
Yes, it would allow for more space in the CES waiver, as the CFC services would not come out of the CES plan.
What are "Attendant Based Services" under CFC?
Attendant Based Services are people in your life who can help with activities of daily living such as personal care, bathing, dressing, cleaning your house, grocery shopping. Within CFC, Consumer-Directed Attendant Support Services (CDASS) allows you to hire an attendant to support you.
The member or authorized representative can support with finding a provider. CFC services do not require having a licensed/skilled nurse or CNA, so you can hire someone you trust and know to help you.
What are the pay rates for CFC ?
Pay rates can be found through HCPF’s Community First Choice Fee Schedule
What is the "Nurse Assessment" being added to the 100.2 process for children receiving CFC and CES Waiver services during their annual renewal?
The Nurse Assessor process is a new process in which a licensed nurse will do a virtual or in person call to assess if skilled services are needed. Then they will submit a service recommendation to the CMA to help figure out what services are needed. This process will launch on 08/01/2025 and CMAs are currently being trained.
